A Poor Man's Plague: Disease and Inequality
Though cholera unified religious communities afflicted by the pestilence, it also heightened socioeconomic inequality and divided populations along class-based lines. In the United States, industrialization caused major cities, such as New York, to experience a massive influx of low wage workers seeking employment. These workers often settled in clustered, densely populated areas that were poorly ventilated. This close proximity of residences coupled with the overflow of waste and fluids contributed to the rapid spread of the disease.
The high concentration of poor citizens residing in run-down, filthy areas resulted in a gradual geographic separation of the working class from their higher-income counterparts. The stigma surrounding poverty drove a wedge between urbanites; the rich began to connect cholera’s spread to the “abject” poverty and “filth and decaying materials” associated with lower socioeconomic classes (Paine, 14).
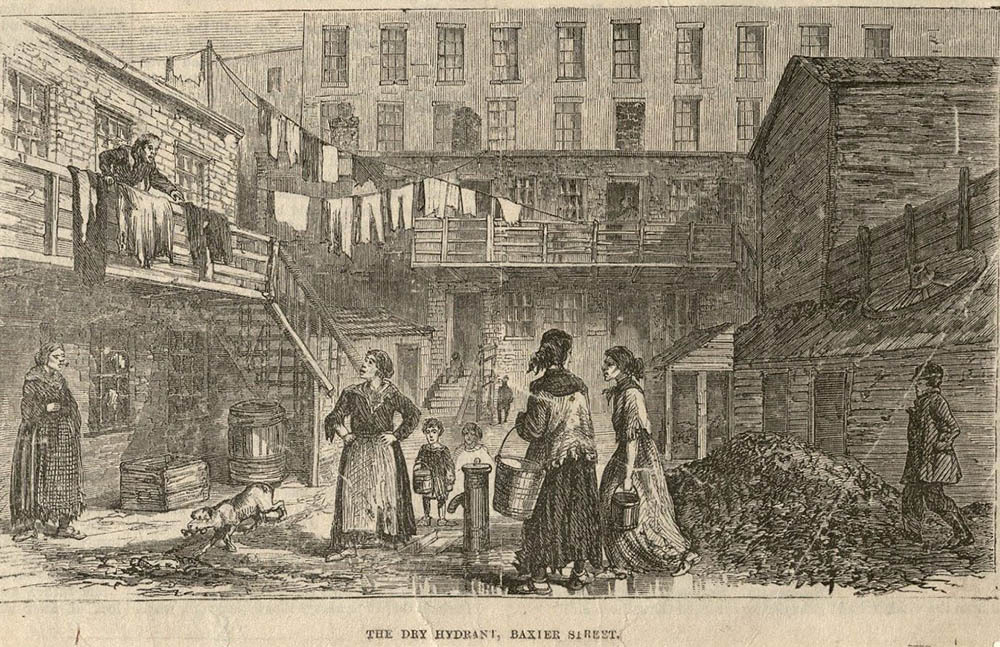
The conditions in which the poor resided in—small, crowded houses; ill-ventilated villages; the “usual evils of poverty”–were thought to induce the spread of cholera (Greenhow, 123; Paine, 14). The “well-nourished, the prudent, and the temperate”, who had the financial means to relocate to rural areas at first sign of the pandemic's arrival on American shores, believed that the infection would only strike the poor, the sinners occupying the slums (Rosenberg, 2009). However, though there was an association between the occurence of cholera and the location of impoverished communities, this did not accurately identify the true biological cause of cholera. But. unfortunately, the damage had already been done: these areas were soon designated the “malarious parts of [the] town” and its inhabitants the “greatest sufferers” from the cholera epidemic (Greenhow, 120; Paine, 10).
This villainization of the poor further exacerbated health care inaccessibility. In New York, officials believed that the clean, well-kept nature of wealthy areas reflected the virtuous nature of its inhabitants, which guarded them against the disease that ravaged poor communities. Since the public believed that the disease targeted sinful populations, as aforementioned, no prioritization or pity was given to the impoverished, obstructing them from receiving care. Such structural and societal barriers prevented lower socioeconomic classes from adopting targeted solutions—such as the purification contaminated water sources and the improvement of living conditions– which would have greatly reduced the number of cholera cases.
The dramatic differences in living areas, diets, and sanitation levels between the lower and upper classes expose the great disparities between city-dwellers. In the cramped neighborhoods of the poor, the dung-hills outside dwellings emitted an “offensive, stithy odour”, demonstrating how poorly adapted the homes were for ventilation (Greenhow, 123). The “old, low [houses] crowded together in narrow lanes and courts” were often in close proximity with industrial complexes characteristic of urbanization, limiting access to pure air (Greenhow, 121). Moreover, diet exposed the reality of disease inequality: garden vegetables and fruits became associated with poverty—and thus cholera—and the “prudent part of [the] population” restricted their diets to consume only “lean fresh meat, potatoes, boiled rice, stale bread, eggs, milk, butter, tea and coffee” (Paine, 14). The lack of cleanliness, adequate lodging, and medical care evidently primed the impoverished for cholera, as epidemics were bound to happen “whenever the population [was] not supplied with the necessaries of life” (Brigham).
This geography of blame portrarying cholera as a “poor man’s plague” built upon pre-existing social tensions between the upper and lower classes of the mid-nineteenth century. Instead of unearthing the true means through which cholera was spread –through contaminated water sources– those who had the power to shape the narrative of the pandemic stigmatized the poor.
Today, as the world battles another pandemic, a familiar narrative emerges: that of scapegoating and blaming populations for the origins of the virus. Alluding to the virus’s origin in Wuhan, China, former president Donald Trump deliberately referred to COVID-19 as the “Chinese virus” and “kung flu”, which worsened already heightened tensions between the United States and ostracized Asian-Americans, who inhabit the liminal space (Moynihan & Porumbescu, 2020). Trump's provocative rhetoric fueled a 150% increase in hate crimes against Asian Americans across the United States (Farivar, 2021). Evidently, scapegoating vulnerable populations becomes common practice in disease outbreaks, as society evades responsibility instead of accepting accountability. Yet time and time again, the implications of sowing division aren't merely reflected in the perpetuation of a disease. The deep division and disruption of social and economic spheres reveals how deep the effects of inequality and disease can percolate.